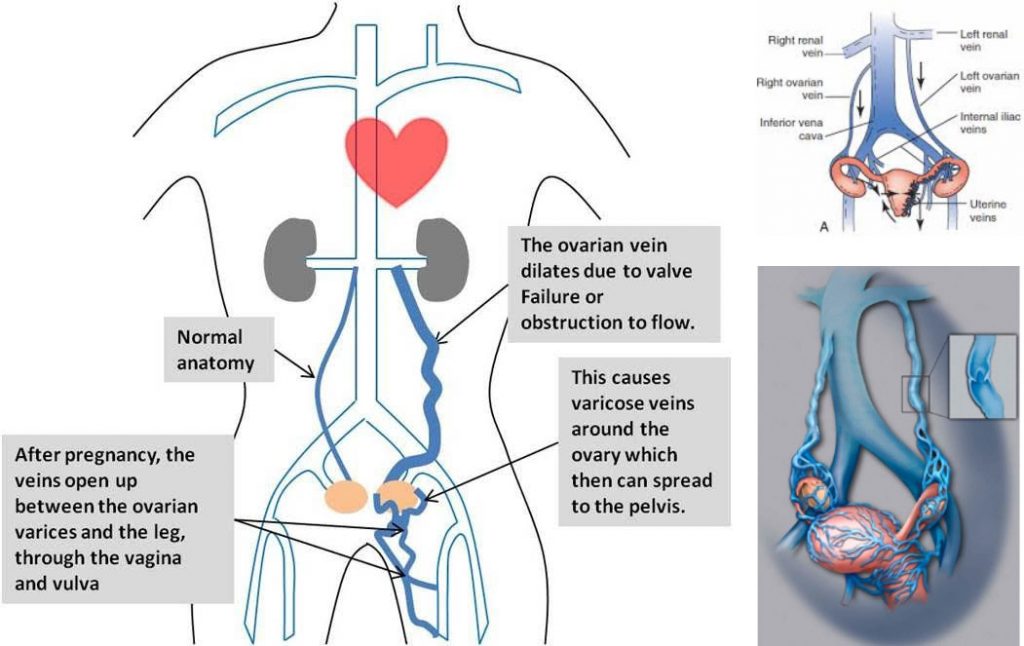
Pelvic congestion syndrome (PCS) is a long term condition due to development of varicose veins in the pelvis that usually affects females more than males. It is not known exactly what population of women suffer from pelvic congestion syndrome however it has been shown that 15% of females in childbearing age are affected with pelvic varicose veins. PCS is a common cause of chronic pelvic pain caused by enlarged ovarian and/or pelvic veins in the lower abdomen, due to backward flow of blood into pelvis veins as a result of faulty valves in the veins. As with the varicose veins in legs, if the valves fail in the pelvic veins, blood that should be pumped out of the pelvis back to the heart, pools and stagnates inside dilated varicose veins within the pelvis. This cause impaired blood flow in the pelvis and make pressure on the pelvic organs such as vagina, bladder or bowel resulting in venous congestion symptoms. The condition may occur or worsen during pregnancy or reproductive age and usually disappears after menopause. The presence of estradiol is believed to be blamed for inducing uterine enlargement with dilatation of the ovarian and uterine veins. PCS can also cause varicose veins in legs leading mainly to atypical varicose veins or to recurrence after surgical treatment.
PELVIC CONGESTION SYNDROME (PCS)
Symptoms and Signs
Pelvic congestion syndrome occurs when varicose veins develop around the ovaries, similar to varicose veins that occur in the legs. The main symptom of PCS is pelvic pain and typically worsens as the day goes on, especially for women who are exposed to long periods of standing or sitting. It also increases with certain activities, such as bicycling and horse riding, and then goes away over the night. In women with pelvic congestion syndrome, pelvic pain lasting more than 6 months often develops during or after a pregnancy and tends to worsen with each pregnancy. Many women of childbearing age have varicose veins in their pelvis, but not all of them have symptoms.
Many times symptoms do not appear until a woman becomes pregnant and then they continue after pregnancy. The following are most commonly reported PCS symptoms:
- chronic pelvic pain or lower back pain that increases after a long periods of standing or sitting and relieved by lying down
- pain during or following sexual intercourse
- pain around menstrual periods
- abnormal bleeding during menstruation and painful menstruation
- frequent urination
- pain in lower legs
- fatigue, constipation and abdominal bloating
- visible varicose veins within the vulva, vagina, inner thigh and sometimes buttocks and legs
- swelling of vagina and vulva
Diagnosis
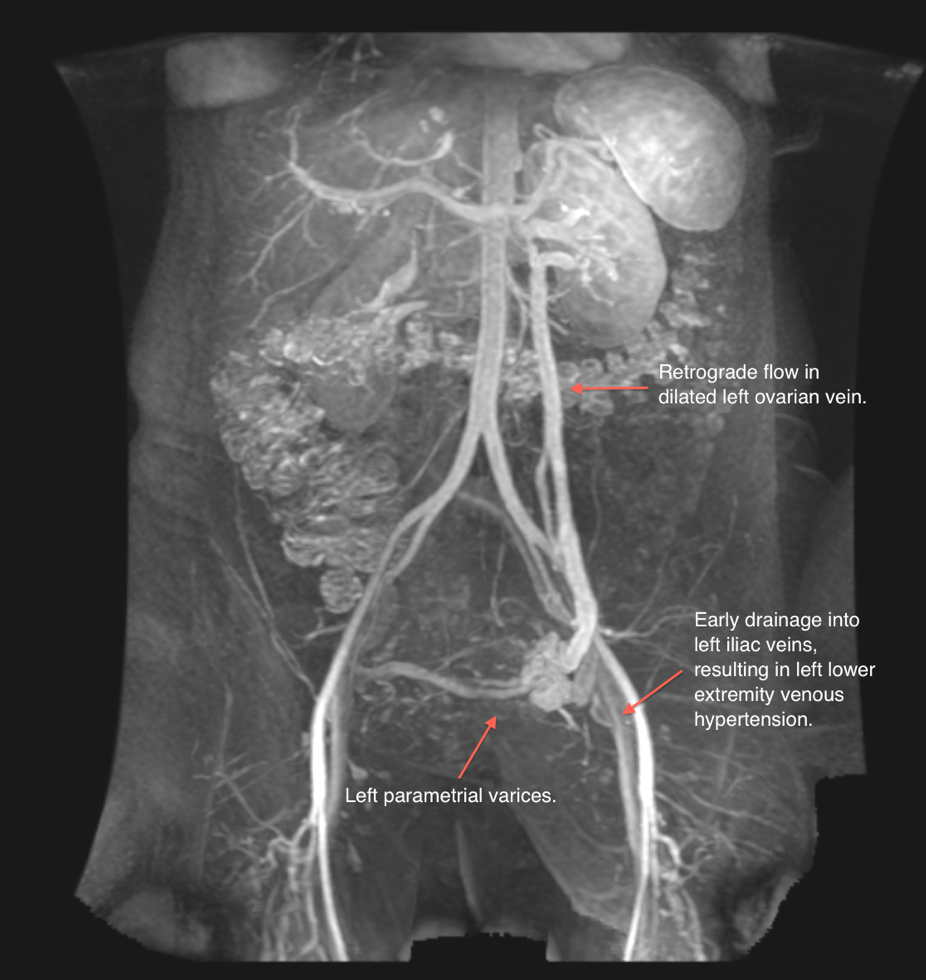
Diagnosis can be made using noninvasive transvaginal Duplex scanning, which provide all the essential information to check for varicose veins in the pelvis and legs in addition to venous reflux assessment. Ultrasound is a diagnostic tool most commonly used and as some research suggested the best study for the diagnosis of pelvic congestion syndrome. However, another imaging test may be needed to confirm the diagnosis. These studies may include phlebography, computed tomography (CT) or magnetic resonance imaging venography (MRI). For doctors to diagnose pelvic congestion syndrome, pain must have been present for more than 6 months and the ovaries must be tender when they are examined. Initial gynecologic examination is mandatory before putting the diagnosis of PCS because most of the above symptoms can be caused by other pelvic diseases (endometriosis, uterine fibroma, pelvic cancer etc.). Good understanding of pelvic venous condition and appropriate investigations including transvaginal duplex ultrasound scanning should be of paramount importance as a great many woman who are suffering from the symptoms of pelvic congestion syndrome are not getting properly diagnosed and treated.
- Trans-vaginal ultrasound is considered a gold standard for diagnosis of dilated veins ad venous reflux (reversed flow) in pelvis
- Computed Tomographic Magnetic Resonance Venography provides visualization of dilated veins and surrounding anatomical structures allowing for treatment plan
- Phlebography with special dye injection provides definitive diagnosis and treatment at the same time
Treatment
- Early medical therapy – Usually include hormonal medications suppressing ovarian functions, flavonoids, nonsteroidal anti-inflammatory drugs and pain killers.
If the above treatment is ineffective, endovascular intervention is an option in order to block blood flow to the varicose veins and prevent blood from accumulating there.
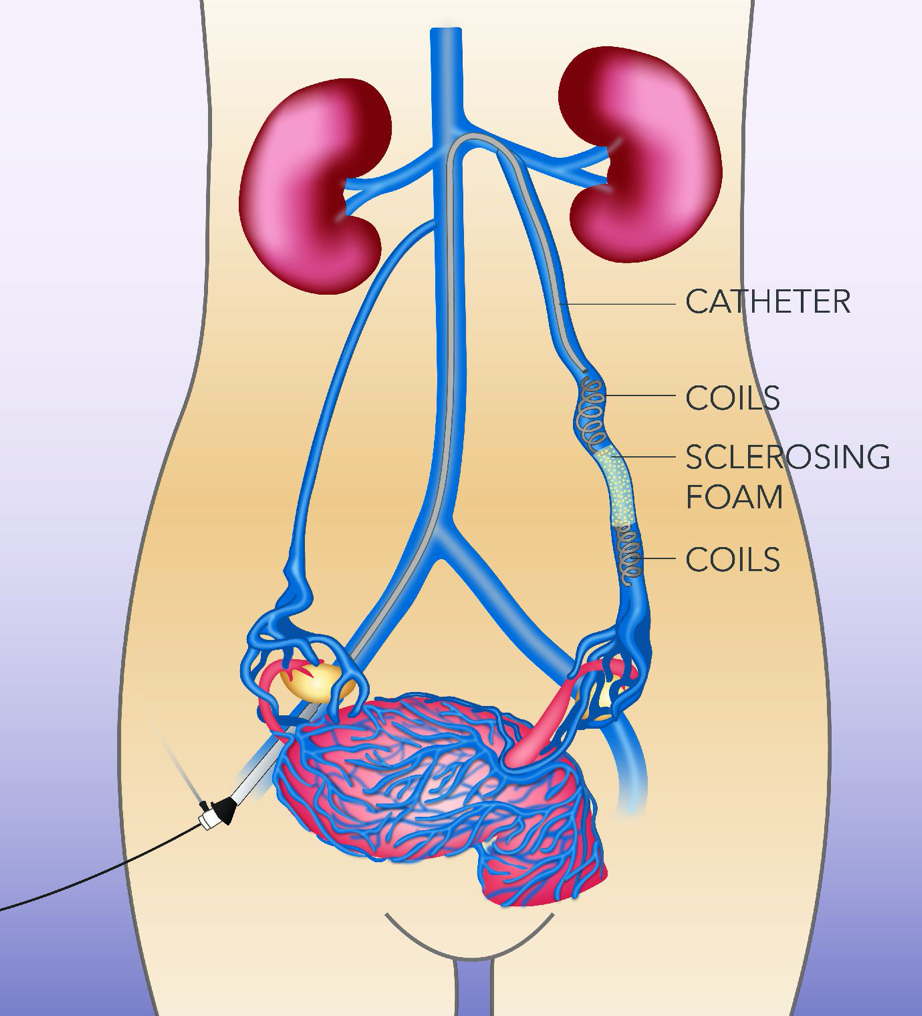
- Embolization of pelvic veins with coils – A minimally invasive endovascular procedure to block ovarian/pelvic vein.After using a local anesthetic to numb access site in the groin, doctors make a small incision through which a thin flexible tube (catheter) is inserted and advanced into the varicose veins. As a result small medical grade spheres called coils are placed into the affected veins blocking the flow of blood and allowing the blood to reroute through healthy veins.
- Foam Sclerotherapy – Similarly, doctors insert a catheter under local anesthesia and inject a solution called Polidocanol or Tetradecyl Sulfate into the varicose veins. This minimal invasive endovascular procedure is usually performed in conjunction with coil embolization. This procedure involves employment of foam that stops blood flow to the varicose
These procedures performed under local anesthesia in Cath lab setting require overnight stay in hospital. Patients report an 80% success rate, as measured by the amount of pain reduction experienced .